
What are shin splints?
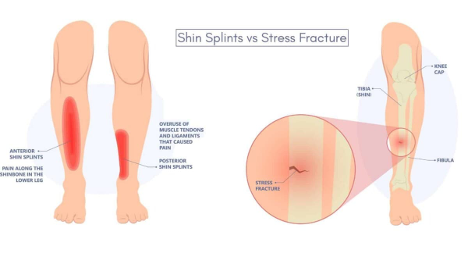
Have you ever felt pain along the front of your shinbone (tibia) that happens during or after exercise? We refer to this as medial tibial stress syndrome (MTSS), or more commonly referred to as “shin splints”.
What causes it?
Shin splints is caused by too much stress on the shinbone and the muscles around it, usually from:
- Doing too much too soon – like suddenly increasing running distance or intensity.
- Running on hard or uneven surfaces.
- Wearing worn-out or unsupportive shoes.
- Poor movement mechanics – like flat feet or poor running form.
- Weak or tight leg and foot muscles.

Pain is caused by inflammation of the periosteum (the lining around the shinbone) because of repeated small impacts or stress. When muscles are weak or fatigued, they don’t support the shinbone properly, so extra pulling force gets placed on the bone with every step, which adds to the pain and stress.
Over time, the repeated impact and stress irritate the bone and surrounding tissues, causing pain and inflammation. If not treated early, it can lead to a more serious issue like a stress fracture (McClure & Oh, 2019).
HOW TO MANAGE:
These are the steps typically recommended to reduce pain, heal the surrounding structures, and prevent recurrence:
Relative rest
Literature recommends “rest” in the acute phase, but for a prolonged period this may not be ideal for athletes (Galbraith & Lavallee, 2009). There are also no specific recommendations on the duration of rest required to ease symptoms, so it is highly dependent on the individual (McClure & Oh, 2019).
Avoid high impact activities such as running and jumping. If pain allows, switching to lower impact activities like swimming and cycling, gives your shinbone time to recover without becoming deconditioned.
Activity Modification & Gradual Return to Sport
After pain has subsided, the goal of treatment should focus on modifying training:
- Decreasing weekly running distance, frequency, and intensity by 50% will likely improve symptoms without needing to stop exercise completely (Galbraith & Lavallee, 2009).
- Follow a walk to run protocol to ease your way back into running (Naderi et al., 2025)
- Avoid running uphills and on uneven surfaces.
Strengthening & Flexibility Exercises
Lower-leg exercises are often recommended for the treatment of MTSS (Naderi et al., 2025)
- Calf raises – keeping the leg straight, push up on your toes to lift the heel
- Eccentric calf raises – Involve lowering the heel over a height slowly after rising up on the toes
- Bent knee calf raises – calf raise with the knees bent
- Calf stretch – Standing with one leg slightly behind the other, lean forward, keeping the back leg straight and heel on the ground to stretch the calf muscles
- Soleus stretch – Standing with one leg slightly behind the other, lean forward, keeping the back leg slightly bent and heel on the ground to stretch the soleus muscle
- Toe curls – scrunching a towel towards you with your toes
- Toe raises – strengthening the tibialis anterior – leaning back against a wall, weight on the heel to lift the toes up
- Banded ankle eversion – With your leg straight and the band pulling from the inside, slowly turn your foot outward like you’re trying to face the sole away from your other foot
- Banded ankle inversion –Sit with your leg straight, tie a resistance band around your foot and anchor it to the side, then slowly turn your foot inward like you’re trying to face the sole toward your other foot.
Strengthen the core and hip muscles (Strakowski & Jamil, 2006)
Core stability:
- Planks (front of side lying)
- Deadbugs – Lie on your back with arms and legs in tabletop position. Alternate extending opposite arm and leg
Hip muscles:
- Glute bridges – Lie on your back with knees bent. Push through heels to lift hips
- Monster walks – Place a resistance band above the knees or at the ankles and walk laterally, keeping tension on the band
- Squats
- Lunges
Proprioception training (balance training) will help the body react to running on incongruent surfaces, key to preventing re injury (Galbraith & Lavallee, 2009). Think wobble boards and one legged stands!
Check Running Form:
Ensure you are running with proper form with a physiotherapist to prevent injury or re-injury.
Footwear:
Athletes should seek out shoes with sufficient shock-absorbing soles and insoles, as they reduce forces through the lower extremity and can prevent repeat episodes of MTSS (Galbraith & Lavallee, 2009).
Individuals with biomechanical problems of the foot (flat feet or over pronation) may benefit from an orthotic (Galbraith & Lavallee, 2009).
Key Takeaways:
Shin splints, or medial tibial stress syndrome (MTSS), are a common overuse injury in runners, often caused by doing too much too soon, poor footwear, or faulty running mechanics. The pain results from inflammation in the lining of the shinbone due to repetitive stress and muscle fatigue. Management starts with relative rest and activity modification, shifting to low-impact exercises like swimming or cycling. A gradual return to running, along with strengthening and stretching exercises for the calves, hips, and core, is essential. Addressing biomechanics, improving balance, and wearing appropriate footwear or orthotics can significantly reduce recurrence and support long-term recovery. If you are struggling with shin splints, book an assessment with a Rise Physiotherapist to start your recovery journey!

